Written by: Becky Beaton-York, PhD
 As a psychologist working closely with clients in chronic pain, I’ve seen how deeply interconnected physical pain and emotional suffering can be. Pain doesn’t just wear down the body, it can cause depression. And in turn, depression can intensify the experience of pain. This bidirectional relationship is more than just a clinical observation; it’s rooted in neuroscience.
As a psychologist working closely with clients in chronic pain, I’ve seen how deeply interconnected physical pain and emotional suffering can be. Pain doesn’t just wear down the body, it can cause depression. And in turn, depression can intensify the experience of pain. This bidirectional relationship is more than just a clinical observation; it’s rooted in neuroscience.
Historically, we referred to this interaction through the lens of Gate Control Theory, which proposed that psychological factors could “open” or “close” gates in the nervous system to modulate pain signals. While this model was groundbreaking at the time, newer frameworks have expanded our understanding.
Today, the Neuromatrix Theory of Pain, introduced by Ronald Melzack, offers a more comprehensive view. It proposes that pain is not a direct output from sensory input alone, but rather a product of a “neuromatrix” in the brain that integrates physical, emotional, and cognitive data to create the experience of pain.
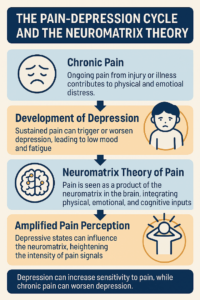
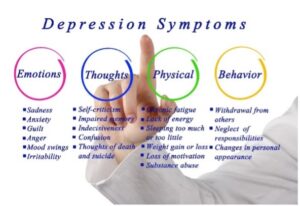
This helps explain why patients with depression often report higher levels of pain. Their emotional state feeds into the neuromatrix, intensifying pain signals even without new or worsening physical injury. Depression can alter neurotransmitter levels (like serotonin and norepinephrine), which not only lower mood but also prime the brain’s pain-processing networks to become more reactive—a process often called central sensitization.
For physical therapists, this has clear implications. A patient who seems “non-compliant” or unusually sensitive to treatment may actually be stuck in a feedback loop where their emotional state affects their physical pain—and vice versa. Depression can slow recovery, reduce motivation for rehabilitation, and increase perceived pain intensity, all of which impact outcomes. Recognizing this, and working in partnership with mental health providers, can be key to effective care.
When physical therapists and mental health providers work together, we can help patients break the cycle. Even small interventions—like validating a patient’s emotional experience, showing compassion, screening for depressive symptoms, or making a gentle mental health referral—can shift the trajectory of healing. Pain and depression are deeply entwined. Recognizing this doesn’t just enhance patient care—it helps patients feel seen and supported in their full experience.
If you would like to learn more about this topic as well as other factors related to health psychology, please check out Dr. Jennifer Steiner’s Healthy Psychology for the Non-Health Psychologists workshops. The Knowledge Tree, A Summit Company, has both a three and a six-hour course on-demand: https://www.theknowledgetree.org/p/health-psychology-online-3-hour
About Summit Professional Education
Summit equips Physical Therapists, Occupational Therapists and SLPs with better continuing education courses that provide CEUs while impacting patient outcomes. Find high-quality on-demand CE along with the largest offering of live options — including live webinars, live streams, and in-person courses. Want to deep dive on a topic? Summit offers hundreds of 6-hour courses for the most in-depth learning!
References:
American Psychological Association. (n.d.). Health psychologists study the intersection of health and behavior. American Psychological Association. Retrieved February 27, 2022, from https://www.apa.org/education-career/guide/subfields/health
Trachsel, L. A., Munakomi, S., & Cascella, M. (2023). Pain theory. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545194/Regis College Libguides+6
